
Allergies can occur in your body but also specifically in your eyes!
When your eye comes into contact with something that it is allergic to such as pollen or cat dander, it may produce an inflammatory response leading to itching, redness or sometimes even swollen eyes. When this occurs, make sure you do not rub your eyes because it can cause the irritation to worsen. Additionally, you should follow up with your eye doctor to consider treatment options such as artificial tears, allergy drops or cold compresses.
The human eye is the organ of sight closely related to the brain and is best compared to a camera. Like a sophisticated camera, the eye has multiple discrete parts which must function together properly to produce clear vision. The function of the eye is to convert light into an electro-chemical signal, which is then transmitted to the brain through the optic nerve. It is in the brain that this signal is converted into “vision.” To illustrate this, we will follow the path that light takes as it travels through the eye and we will discuss the various ocular structures encountered along the path.

Cornea
The first surface encountered by a ray of light is the tear film. The eye’s surface must be kept moist at all times. To achieve this, glands in and near the eyelids produce both tears and a special oil, which mix together and coat the eye. This tear film coats the cornea, which normally is the crystal clear window to the eye. Deficiencies in tear production (dry eyes) can impair vision and cause redness or discomfort. Behind the cornea, we enter a space called the anterior chamber, which is filled with fluid called the aqueous. The aqueous humor is normally clear like water and is responsible for maintaining the pressure of the eye. Disturbances in the production or drainage of the aqueous can result in high pressure in the eye and even glaucoma.
Iris (Eyes)
Inside the anterior chamber is the iris. This is the part of the eye that is responsible for one’s eye color. It acts like the diaphragm of a camera, dilating and constricting the pupil to allow more or less light into the eye.
Lens
The next structure we encounter is the crystalline lens. The lens is responsible for focusing light onto the retina. It changes shape slightly to allow us to change focus between objects that are near and those that are far. As we age, the lens of the eyes becomes less flexible and unable to “accommodate” or change focus as well. This is called presbyopia. When a patient becomes presbyopic, they will often need to wear reading glasses or switch to multi-focals. Eventually, the lens of the eyes loses its original clarity and can become yellowish or cloudy. This is called a cataract and degrades the quality of the image focused on the retina. When the cataract becomes dense enough to interfere with vision, it can be replaced with a clear artificial lens implant during cataract surgery.
Vitreous Humor
Next in our voyage through the eye is the vitreous. This is a jelly–like substance that fills the body of the eye. It is normally clear. In early life, it is firmly attached to the retina behind it. With age, the vitreous becomes more water–like and may detach from the retina. Often, little clumps or strands of the jelly form and cast shadows, which are perceived as “eye floaters.” While frequently benign, sometimes floaters can be a sign of a more serious condition such as a retinal tear or detachment and should be investigated with a thorough eye examination (see retinal detachment).
Retina
Finally, light reaches the retina, a thin tissue lining the innermost wall of the eye. The retina acts much like the film in a camera. The retina responds to light rays hitting it and converts them to electrical/chemical signals carried by the optic nerve to the brain. The outlying parts of the retina are responsible for peripheral vision while the center area, called the macula, is used for fine central vision and color vision. The very center of the macula is called the fovea. It has a very high concentration of special cells called cones, which make it the only part of the retina capable of 20/20 vision. Any disease that affects the macula, such as macular degeneration, will result in a decrease in straight ahead central vision.
Retinal Layers
Like film, the retina is composed of several layers with different roles. The first layer encountered by light is called the nerve fiber layer. Here, the nerve cells travel from all the parts of the retina to the optic nerve. Under this layer are most of the retinal blood vessels. They are responsible for nourishing the inner parts of the retina. The outermost layer is the photoreceptor layer. The photoreceptor layer, composed of cones for fine and color vision, and rods for vision in dim light, consists of the cells that actually convert light into nerve impulses. There are approximately 120 million rods and 6 million cones in a human retina. Most of the cones are located in the macula. The photoreceptor cells lie on top of a layer of cells called the retinal pigment epithelium or RPE. The RPE is responsible for keeping the photoreceptors healthy and functioning well. Under the RPE is the retina’s second set of blood vessels, which are in a layer called the choroid. The RPE, fed by the blood vessels of the choroid, nourish the photoreceptors.
The optic nerve is the structure which takes the information from the retinas and delivers it to the brain, where this information is interpreted as a visual image. The optic nerve consists of a bundle of about one million nerve fibers. The position in the back of the eye where the nerve enters the globe corresponds to the “blind spot” since there are no rods or cones in this location. Normally, a person does not notice this blind spot because of its off-center location and rapid movements of the eye which allow the brain compensate for this absent information. In glaucoma, the nerve becomes damaged often due to high pressure within the eye.
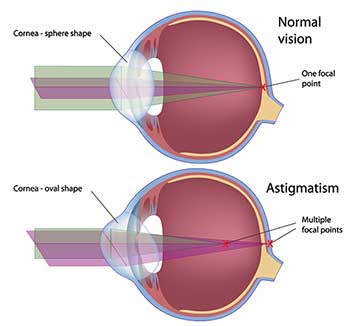
Astigmatism is a part of your glasses prescription. It is a very common condition and is nothing to be feared! It simply means that instead of your eyes being shaped spherically like a soccer ball, they are shaped more like a rugby instead. When this occurs you need slightly more prescription in one portion of your eye than the other. Your eye doctor will be able to test and treat for this with either glasses, contacts or even refractive surgery (eg. LASIK).



A cataract is a clouding of the normally clear lens of the eye. For people who have cataracts, seeing through cloudy lenses is a bit like looking through a frosty or fogged-up window. In fact, cataract means waterfall and that is how the condition got its name; people felt like they were looking through a waterfall. Clouded vision caused by cataracts can make it more difficult to read, drive a car (especially at night), or see the expression on a friend’s face.
Most cataracts develop slowly and will not disturb your eyesight early on. With time, cataracts will eventually interfere with your vision; however, it is easy to correct with a simple procedure.
At first, stronger lighting and eyeglasses can help you deal with the changes cataracts cause. If impaired vision interferes with your usual activities, you might need cataract surgery. Fortunately, cataract surgery is generally a safe, effective procedure.
Myopia, commonly known as nearsightedness, is the most common refractive error. People with myopia have difficulties seeing distant objects. It can either occur when the eyeball is too long or if the cornea or lens is too curved.

Causes:
If a child possess progressive myopia, it may lead to retinal complications and reduced vision when they are older.
Atropine Eye Drops
We provide atropine treatment for myopia in children. Although atropine drop is approved by FDA for treating amblyopia (lazy eye), studies have reflected that myopia progression can be minimized with atropine eye drops. For child with mild and moderate myopia, low dose atropine eye drops would be prescribed. These drops are applied at night before sleep so that your child would not be affected by the side effects, including blurred vision and worsened light sensitivity, during the day. Plus, these side effects are usually too mild for child to notice.
When child start atropine therapy, we will schedule follow-ups with the schedule below:
The follow-up schedule could be adjusted if any complications arise.
Soft Contact Lenses
We offer MiSight® 1 day contact lens, which is the first FDA-approved soft contact lens, is designed to lessen the progression of myopia and correct vision in children aged 8-12 years old at the initiation of treatment. It helps children see distant objects, somehow like wearing glasses, so that they can engage in the activities at school. Most importantly, the lenses are so soft and comfortable that can be easily put in and taken out for children. The lenses should be worn every day and discarded after each removal.
As convenient as contact lenses are, it is very important to remember that they are a FDA approved medical device. Therefore, it is important to take proper care and handle your contact lenses safely.
If you overwear your contact lenses (ie. sleeping in them when advised not to) or clean and handle them improperly, it could lead to red eyes, infections or even ulcers. If any of those things become severe, they can even lead to blindness!


Therefore, whenever you are using your contact lenses, make sure you are throwing them out at the proper time. For example, even if you open a monthly lens and only use it three times, it is still important to throw them out at the end of the month. Also ensure that you are cleaning them with your doctor’s prescribed cleaning solution and making sure that they soak in the solution for the proper amount of hours.
If you have any questions make sure to contact your eye doctor!
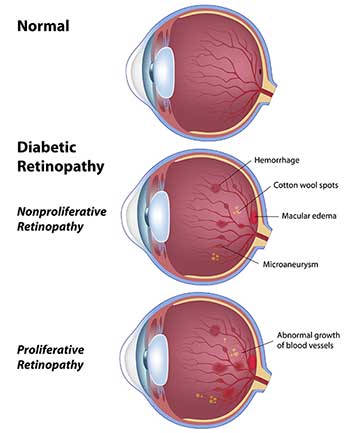
If you have been diagnosed with diabetes, it is important to follow up with your eye doctor routinely. This is because if your diabetes is not well controlled or if you have had diabetes for many years, you are at risk of developing bleeding in the back of the eye. If it gets severe enough it may cause reduced vision from bleeding, glaucoma, or even large cataract formation.
There is no treatment for diabetic changes that are mild apart from good blood sugar control; however, if the bleeding is severe enough it may need medication injections.
Therefore, make sure to follow up with your eye doctor consistently when you have diabetes.


What is dry eye syndrome?
Dry eye syndrome is a common problem that can range in severity from mild to severe. This is caused by a disruption of the tear layer that normally coats the surface of the eye. Symptoms include:
What causes dry eye syndrome?
Causes include:
What tests can look for dry eye syndrome?
Tests can be done in the office including looking at eye sensation, tear layer stability, damage to the surface of the eye, tear production, and eye inflammation. A blood test can also be performed to look at autoimmune associated dry eye and Sjogren’s syndrome.
What is the management for dry eye syndrome?
Depending on the case, different treatments for dry eye syndrome are used including:
Hyperopia is when you can see the distant object clearly (depending on the prescription) but your near vision may be a little bit blurry. This can be corrected with glasses, contacts or surgery.
When children are first examined for their farsightedness, They may need an extra eye drop that will allow the doctor to produce a more accurate prescription. This is because some children’s eyes are constantly working hard to accommodate for their prescriptions. Therefore, the drop known as cyclopentolate can be a very important part of the examination to let us know their exact prescription.

Floaters are little black dots or lines that float in front of your vision.
Flashes are flashes of light that may happen in one or both eyes either in front of your eyes or to the side of your vision.
Both can be a normal finding for older patients or patients with higher prescriptions; however, they may also be indicative of a larger retinal issue. Therefore, if you notice any new floaters or flashes definitely make an appointment with your eye doctor soon!
Glaucoma is not just one eye disease, but a group of eye conditions resulting in optic nerve damage, which causes loss of vision. Abnormally high pressure inside your eye (intraocular pressure) usually, but not always, causes this damage.
Glaucoma is the second leading cause of blindness. Sometimes called the silent thief of sight, glaucoma can damage your vision so gradually you may not notice any loss of vision until the disease is at an advanced stage. The most common type of glaucoma, primary open-angle glaucoma, often has no noticeable signs or symptoms.

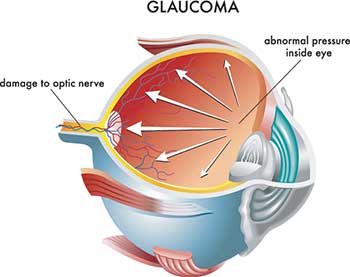
Early diagnosis and treatment can minimize or prevent optic nerve damage and limit glaucoma-related vision loss. It’s important to get your eyes examined regularly, and make sure your eye doctor measures your intraocular pressure.
If you are noticing that you are unable to wear your contacts for as long as previously due to discomfort or notice that there is mucous discharge this may be due to giant papillary conjunctivitis.
GPC is the eye’s allergic reaction to either an overworn contact lens or its deposits. Your eye doctor can help treat it with either allergy drops or a low dose steroid eye drop.
If you are having any of these complaints make sure to follow up with your local eye doctor!


If you have been diagnosed with hypertension it is very important to follow up with your eye doctor due to the possibility of changes to the retinal blood vessels or even your optic nerve! If you notice your vision is getting blurry, make an appointment with your eye doctor because this may be due to the hypertension as well.
Keratoconus is an eye condition that causes the front of your eye (cornea) to become steeper. As the keratoconus progresses, the cornea becomes steeper, changing it from its normal round shape to more of a cone shape and causing it to protrude out. When this occurs, your vision may become very blurry.
Initial treatment for the mild form of the disease is to provide glasses; however, people with more progressed keratoconus may need hard contact lenses such as gas permeable (smaller) or scleral lenses (larger). Additionally, if the keratoconus is progressing you may need a surgical procedure called cross-linking to strengthen the cornea and to reduce the progression of the keratoconus.


What is laser vision correction?
Laser vison correction is a method of correcting the vision for myopia, hyperopia, astigmatism and presbyopia. The treatment is applied to the cornea on the surface of the eye. In people who are nearsighted or myopic, the treatment reduces the curvature of the cornea that is too steep, and this brings images in focus on the retina. In people who are farsighted or hyperopic, the treatment results in a steeper cornea to increase the eye’s focusing power. In astigmatism, the treatment smooths the cornea to make it more regular. Refractive surgery can be a good option in people who:
The most common methods of refractive surgery include LASIK (laser in situ keratomileusis) and surface ablation or PRK (photorefractive keratectomy). LASIK involves creating a flap, applying laser to the cornea and then replacing the flap. Surface ablation involves removing the surface layer, applying the laser to the cornea and the often placing a contact lens to help the surface heal. If you are considering refractive surgery, you and your ophthalmologist can discuss the best treatment to suit your vision needs and your lifestyle.
What are the alternatives to refractive surgery?
Alternatives to laser refractive surgery include wearing glasses or contacts, other cornea surgery to correct the vision or placing an intraocular lens to correct the vision.
The high success rate of LASIK and laser vision correction can be attributed to the advanced technology available today as well as the thorough evaluation process by which candidates are selected for the procedure.
Please call the office to make an appointment for a laser vision correction consultation.
The macula is a structure in the back of your eye that helps you see. As you grow older there may be some waste products that build up in the macula. As more waste products build up it may lead to blurry vision or may cause fluid to accumulate under the macula if it becomes very severe.
Macular degeneration occurs more so in Caucasian or Asian patients.
Treatment for macular degeneration varies depending on what stage you have and may include vitamins or simply a healthy diet filled with lots of leafy greens. If the disease progresses to a severe condition you may also need medication injections to control it. It is always important to not smoke because smoking can make the condition progress rapidly.


Myopia is a common ocular condition that can be treated with glasses, contacts or surgery.
Children show the largest progression of myopia in their lifetime. If you notice your child is progressing in myopia more than normal we may need to consider some myopia control treatments such as low dose atropine eye drops or specialty contact lenses. It is also important to improve time outdoors and to take breaks during periods of near work. Myopia is a disease that can lead to severe complications when patients are older such as retinal detachments, glaucoma or macular scarring. Therefore, if we can reduce myopia now we can preserve the child’s vision in the future.
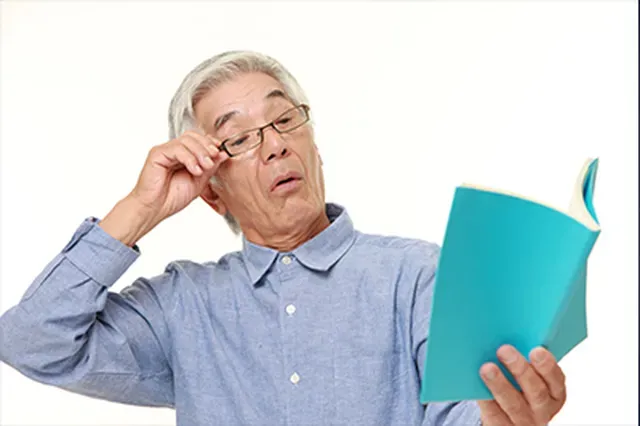
As we get older, our ability to see up close gradually diminishes. This is known as “presbyopia.” This usually occurs around age 40 but the specific timing may differ depending on a multitude of different factors.
The best treatment for presbyopia is reading glasses. Therefore, if you think your reading vision is getting more and more blurry and you are around 40 years old, definitely make an appointment with your eye doctor now.

Retinal detachment affects approximately 1 in 10,000 people each year. If left untreated, most retinal detachments will lead to loss of vision. An understanding of some of the normal anatomy of the eye may be useful in understanding how retinal tears and detachment occur and the symptoms which they may cause.
The retina is a thin tissue that lines much of the inside of the eye. The center portion of the retina is called the macula. The macula is responsible for fine central vision and for color vision. The more peripheral parts of the retina provide peripheral vision. The vitreous is a jelly-like substance, which fills the center of the eye. The vitreous is normally clear and as such will normally not affect vision. The vitreous is attached to the retina in many areas.
In some regards, the way in which the eye works may be compared to a camera. In a camera, light is focused by the lens onto a film, where an image is formed. In the eye, the cornea (a clear structure forming part of the front wall of the eye) and the lens focus light onto the retina where an image is formed. The retina then converts this image into neural signals, which are transmitted to the brain.
Floaters, flashing lights and posterior vitreous detachment
When we are young, the vitreous is normally a clear structure which does not affect our vision. As we age, however, changes may occur within the vitreous. Some parts of the vitreous may become more liquefied; other parts of the vitreous may condense and start to shrink. As the vitreous shrinks it may pull away from its attachments to the back part of the eye. This separation of the vitreous from its attachments to the back part of the eye is called a posterior vitreous detachment. Posterior vitreous detachments occur as a normal aging event but may be more common or occur earlier in people who are nearsighted (myopic), have undergone cataract surgery or who have had eye trauma or inflammation.
As a result of these changes within the vitreous, small clumps or strands may develop in the vitreous. As light passes through the vitreous, these small clumps or strands may cast shadows on the retina. We see these shadows as floaters. Although the floaters appear to us to be outside of the eye, they are actually within the eye. The floaters can have many different shapes. While most often they appear as dots or lines, sometimes they can also appear like circles, clouds, cobwebs or even like a spider or a fly. Most of the time, these objects will appear to move. Floaters can also be caused by bleeding or inflammation in the eye.
The vitreous pulling away from the retina can also cause the sensation of seeing flashing lights. These sometimes appear like “lightening streaks” in the eye. The sensation of flashing lights is not, however always a sign of the vitreous pulling on the retina. Other conditions such as a migraine can also cause the sensation of seeing flashing lights.
At times, a posterior vitreous detachment may occur without associated symptoms. While most posterior vitreous detachments do not lead to more serious problems, sometimes a retinal tear or detachment may arise as a result of a posterior vitreous detachment. Because of the risk of there being an associated retinal tear or detachment, anyone having the new onset of floating spots or flashing lights should undergo a careful retinal evaluation.
Retinal tear and detachment
As the vitreous pulls away from the retina during a posterior vitreous detachment, the retina may at times tear. Retinal detachment occurs if fluid from within the vitreous passes through the tear and collects under the retina, causing the retina the separate from the underlying tissue (retinal pigment epithelium). The retinal tear may be associated with the symptoms of a posterior vitreous detachment (flashing lights and floaters). However as most retinal tears occur in the more peripheral parts of the retina, a retinal tear will usually not cause loss of vision unless there is progression to retinal detachment. The detached retina is not capable of normal sight and as the retinal detachment enlarges and approaches the central part of the retina there will be an enlarging area of vision loss. This is sometimes described as a shadow or veil covering the vision. Sometimes retinal tears occur without associated floaters or flashing lights. In these cases, the first symptoms to occur may be the loss of vision due to retinal detachment.
Not all retinal tears will lead to retinal detachment. At times, a retinal hole or tear may be found during a routine eye exam without there having been any associated symptoms. In this situation, the risk of progression to retinal detachment may be low and treatment of the retinal tear in this situation may not always be needed. However, retinal tears associated with symptoms suggesting that there has been a recent posterior vitreous detachment are usually felt to be of high risk of progression to retinal detachment and should, under most circumstances be treated in order to minimize the risk of progression to retinal detachment. Retinal tears, if detected early, can usually be treated in such a way as to avoid retinal detachment.
Treatment of Retinal Tears
Retinal tears can be treated using either laser photocoagulation or cryotherapy. Laser photocoagulation is a procedure where a special light is directed to the retina and used to create burns in the retina surrounding the retinal tear. Cyrotherapy is a procedure where a freezing probe is placed on the surface of the eye and used to create a freeze extending to the retina surrounding the retinal tear. Whether laser photocoagulation or cryotherapy is used, as the eye heals a scar will form sealing the retinal tear and in most cases preventing a retinal detachment from occurring. Both laser photocoagulation and cryotherapy are usually performed in the doctor’s office. Treatment of retinal tears is usually successful in preventing retinal detachment. Unfortunately, occasionally even after treatment of a retinal tear, retinal detachment may still occur. Therefore, if any new symptoms arise following treatment of a retinal tear, the retina should be re-examined and even in the absence of new symptoms, continued follow-up after treatment of a retinal tear is needed.
Treatment of Retinal Detachment
Some retinal detachments, if diagnosed when the detachment is small, may be treatable with only laser photocoagulation or cryotherapy. More often, however, if retinal detachment occurs, more extensive surgery is usually needed. The surgical procedures, which are frequently used for repair of retinal detachment, include pneumatic retinopexy, scleral buckle and vitrectomy.
When pneumatic retinopexy is used for repair of a retinal detachment, a gas bubble is injected into the vitreous cavity. The patient is then positioned in such a way so that the gas bubble pushes against the retinal tear and temporarily seals the tear, which has caused the retinal detachment. With the retinal tear covered by the gas bubble, the fluid that has accumulated under the retina will usually be reabsorbed by the eye within one or two days. As the gas bubble will also be reabsorbed by the body, it is necessary to also create a more permanent seal surrounding the retinal tear. To create this permanent seal, pneumatic retinopexy is done in conjunction with either retinal cryopexy or laser photocoagulation. Sometimes the retinal cryopexy will be done prior to the injection of the gas bubble. On other occasions, however, the cryopexy or laser photocoagulation will be done on a subsequent day, after there has been clearing of the subretinal fluid. Depending on which gas is used, the bubble takes between two and six weeks to be cleared from the eye. Pneumatic retinopexy can usually be performed in the doctor’s office. While pneumatic retinopexy is a good option for the repair of many retinal detachments, not all retinal detachments are suitable for this type of repair.
Scleral buckling surgery is another good option for repair of many retinal detachments. In scleral buckling surgery a buckling element, usually a piece of silicone, is sutured to the sclera (the outer wall of the eye) in such a way as to indent the wall of the eye. This indentation reduces the traction that is created by the vitreous pulling on the retinal tear, thereby allowing the tear to close. Cryotherapy is usually used in this procedure as well, to create a permanent seal surrounding the retinal tear. The fluid which has collected under the retina is either surgically removed or is allowed to spontaneously reabsorb. Sometimes a gas bubble will also be injected into the vitreous cavity as part of this procedure. Scleral buckling surgery is performed in an operating room. It is frequently done under local anesthesia and the patient will usually return home the same day as the surgery.
Sometimes, particularly in more complicated retinal detachments; it may be preferable or necessary to remove the vitreous in order to reattach the retina. This procedure is called a vitrectomy (also called pars plana vitrectomy). Vitrectomy may be used in combination with the other techniques already described. During vitrectomy surgery, small incisions are made through the sclera, which allow microsurgical instruments to be introduced into the vitreous. The vitreous, along with any scar tissue, which may also be present, is removed. In this way the traction on the retina is eliminated. The fluid that has collected under the retina is surgically removed. The vitreous cavity is then usually filled with a gas bubble. Sometimes in more complicated retinal detachments the vitreous cavity may instead be filled with silicone oil. The retina tear is surrounded with laser photocoagulation. A scleral buckle may be placed in conjunction with vitrectomy. Vitrectomy surgery is performed in an operating room. The patient will usually return home the same day as the surgery.
The choice of which of these procedures is most appropriate for the repair of a retinal detachment is dependent on many factors. These include the location of the responsible retinal tears and the presence or absence of scar tissue on the retina (proliferative vitreoretinopathy). The decision of which method of retinal detachment surgery is best can only be made after a careful evaluation. Fortunately, with these techniques, it is possible to successfully repair most retinal detachments. While most retinal detachments are successfully repaired with a single operation, in some cases more than one operation may be needed.
The amount of vision recovered after successful retinal detachment surgery is variable. The most important factors influencing the postoperative vision are whether the macula is detached prior to surgery and the duration the detachment has been present. If retinal detachment surgery can be done before the detachment has extended to the macula (the center portion of the retina which is responsible for central vision) the likelihood of maintaining good central vision is excellent. In many cases, however, a retinal detachment may not be detected until after the central vision is affected. If the macula is detached prior to the surgical repair, there is usually some permanent vision loss even after successful retinal detachment surgery. While it is common to obtain some improvement in vision shortly after surgery, the final best vision may at times take 6 months, a year, or even longer to obtain.
Vision loss can be in the center or in the periphery of your vision. There are many possible causes of vision loss, including:
These possible eye conditions are for reference only and do not contain all possible conditions. If you have any unusual vision symptoms, speak with your ophthalmologist. Early detection is the best way to keep your eyes healthy. Many cases of vision loss are preventable and treatable.
